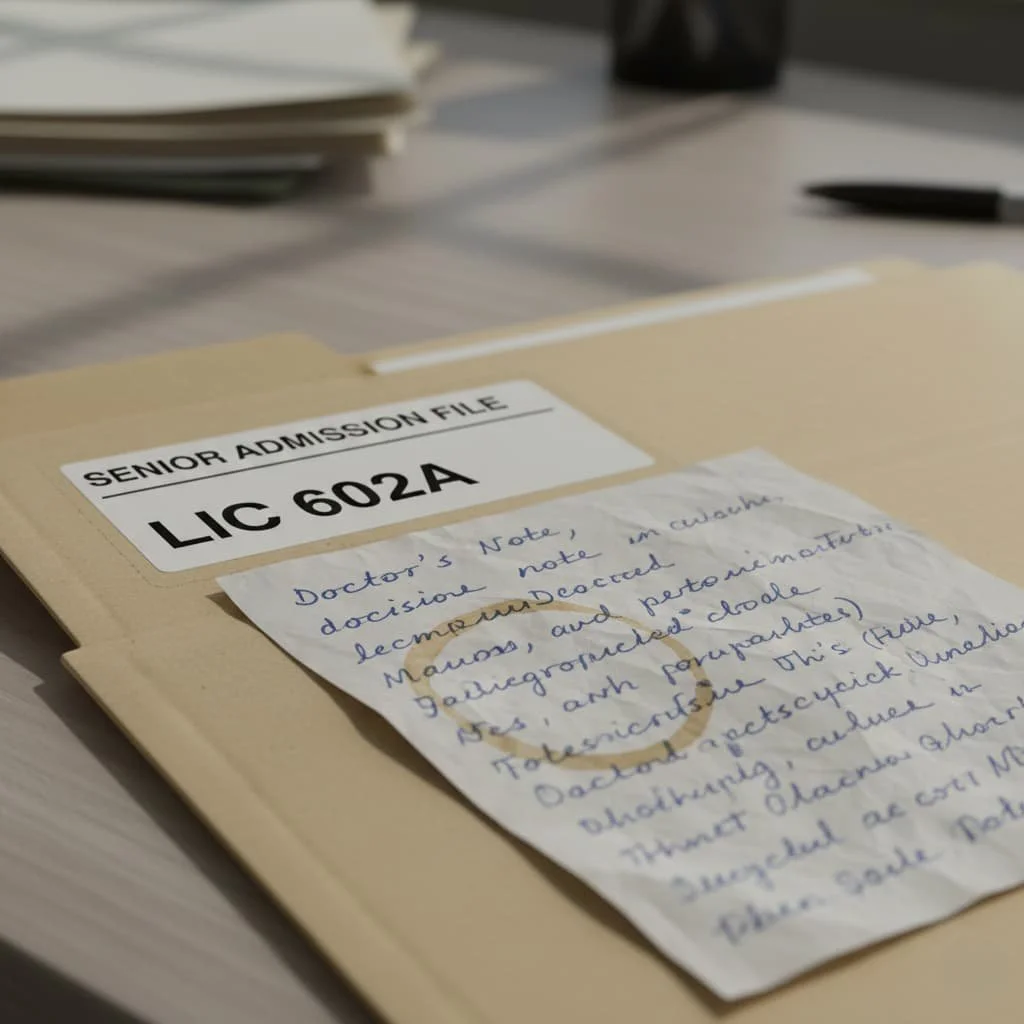
Illegible Doctor Notes: The Hidden Liability Threatening Timely Care Admission
Image generated with AI for illustrative purposes only.
The LIC 602A Form (Pre-Admission Health Status Report) is a critically important document. It serves as a guarantee that a specialized care facility (such as a Residential Care Facility for the Elderly, RCFE) can safely and adequately meet the needs of a new resident.
However, a serious and common issue jeopardizes this process: unreadable doctor notes. A single unclear line, an incomprehensible abbreviation, or rushed handwriting can stall the entire admission process, causing stress, wasting time, and, most importantly, putting the resident's well-being at risk.
Understanding the LIC 602A Form
What is this document? The LIC 602A is completed by a licensed healthcare professional to confirm a patient's current health status, diagnoses, and care needs prior to admission into a care facility.
Legal Significance: The form is often a mandatory licensing requirement. It serves as proof that the facility has conducted the necessary due diligence and is legally authorized to provide the required level of care.
Why Doctor Notes Are Critical: Patient Safety Risks
For the staff reviewing the admission, a diagnosis alone is not enough. They require clinical clarity:
Need to Know How to Care: Reviewers look for precise information on specific procedures, diets, or assistance required.
Assumptions Are Forbidden: If a note is illegible or ambiguous (e.g., "SPEC. DIET" without explanation), the facility is not allowed to guess the meaning. Due to the high risk to patient safety, any ambiguity immediately halts the process.
The Problem: Illegibility and Safety Hazards
Unreadable records are not just an inconvenience; they are a proven threat to patient safety, as highlighted by health research:
Risk of Medication Errors: Illegible handwriting in prescriptions is a known cause of medication errors, which can have severe consequences (NIH/ResearchGate, ISQua).
Increased Staff Workload: Unclear notes force nurses and administrators to spend time deciphering them, diverting attention from direct care duties (NIH).
Impact on Care Continuity: Illegible handwriting hinders the transfer of vital information between different clinicians involved in the patient's care.
Common Reasons Doctor Notes Become Unreadable
Handwriting Issues: The classic factor—rushed or poor handwriting.
Haste and Abbreviations: A physician under time pressure may use non-standard abbreviations or medical jargon unfamiliar to the care facility staff.
Poor Transmission Quality: Even a perfectly written document can become unreadable due to low-resolution scanning, poor fax quality, or shadows on the copy.
How Unreadable Notes Trigger Admission Delays
Any ambiguity in the LIC 602A form initiates a chain of delays:
Requests for Clarification: The reviewer must put the form aside and begin the time-consuming process of requesting clarification, which often takes hours or even days.
Bureaucratic Bottlenecks: Getting a response from an overburdened doctor's office requires time, while the patient is waiting for placement.
Lost Placement Opportunities: The delay may cause the facility to accept another admission-ready patient, leading to the family losing their desired placement spot.
The Costs of Delays: Financial and Emotional
Additional Expenses: The patient may remain in a hospital setting longer than medically necessary, which can incur additional expenses.
Health Risks: Postponing specialized care can worsen the patient’s condition or delay their stabilization.
Stress on Families: A lengthy, uncertain admission process creates significant emotional strain on the patient and their loved ones.
Best Practices to Improve Readability
Healthcare research consistently points to the shift toward digital documentation as the key solution:
| The Problem | The Solution | Source |
|---|---|---|
| Illegible Handwriting | Adopt Electronic Health Records (EHR) and use typed text | MEDcury, ResearchGate |
| Vagueness and Gaps | Use specific, objective language and fill all fields | CMS, IntelyCare |
| Risk of Misinterpretation | Use standardized abbreviations only and aim for digital compliance | AHIMA, ResearchGate |
Actionable Recommendations:
For Physicians: Whenever possible, use typed notes. If handwriting is necessary, write as clearly as possible, avoiding non-standard abbreviations.
For Facilities: Implement an internal pre-review checklist to check the legibility and completeness of the form before final approval.
For Families and Agencies: Act as "gatekeepers." Review the document for obvious ambiguities before sending it to the facility.
The Future: Transparency and Technology
Research, including that from Kaiser Permanente, shows how using modern technology eliminates many issues:
EHRs: Completely eliminate the handwriting problem.
Transparency (OpenNotes): When patients can view their records, clinicians are encouraged to maintain more accurate and understandable documentation, enhancing safety.
Artificial Intelligence (AI): Using Natural Language Processing (NLP) systems can standardize notes and detect errors caused by jargon and grammatical issues.
Conclusion
Readability is not optional; it is a safety requirement. An unreadable doctor's note, no matter how small, can halt the placement process, cause financial strain, and introduce unnecessary risk to a vulnerable patient's health.
Understanding and addressing this single small flaw by ensuring clear, preferably digital, documentation is the most effective way to prevent major delays and guarantee a safe, timely transition to the required care.
List of References
"Handwriting Legibility and Medical Errors". Source: National Institutes of Health (NIH), 2018–2024.
"Requirements for Documentation and Medical Records in Skilled Nursing Facilities". Source: Centers for Medicare & Medicaid Services (CMS), Code of Federal Regulations, 2024.
"The Role of Electronic Health Records (EHRs) in Patient Safety". Source: Centers for Disease Control and Prevention (CDC), 2023.
"Patient Access to Electronic Health Records and Documentation Quality". Source: Kaiser Permanente Division of Research, 2022.
"Guidelines for Clinical Documentation and Standardized Abbreviations". Source: Mayo Clinic / Professional Associations (e.g., AHIMA), 2023.