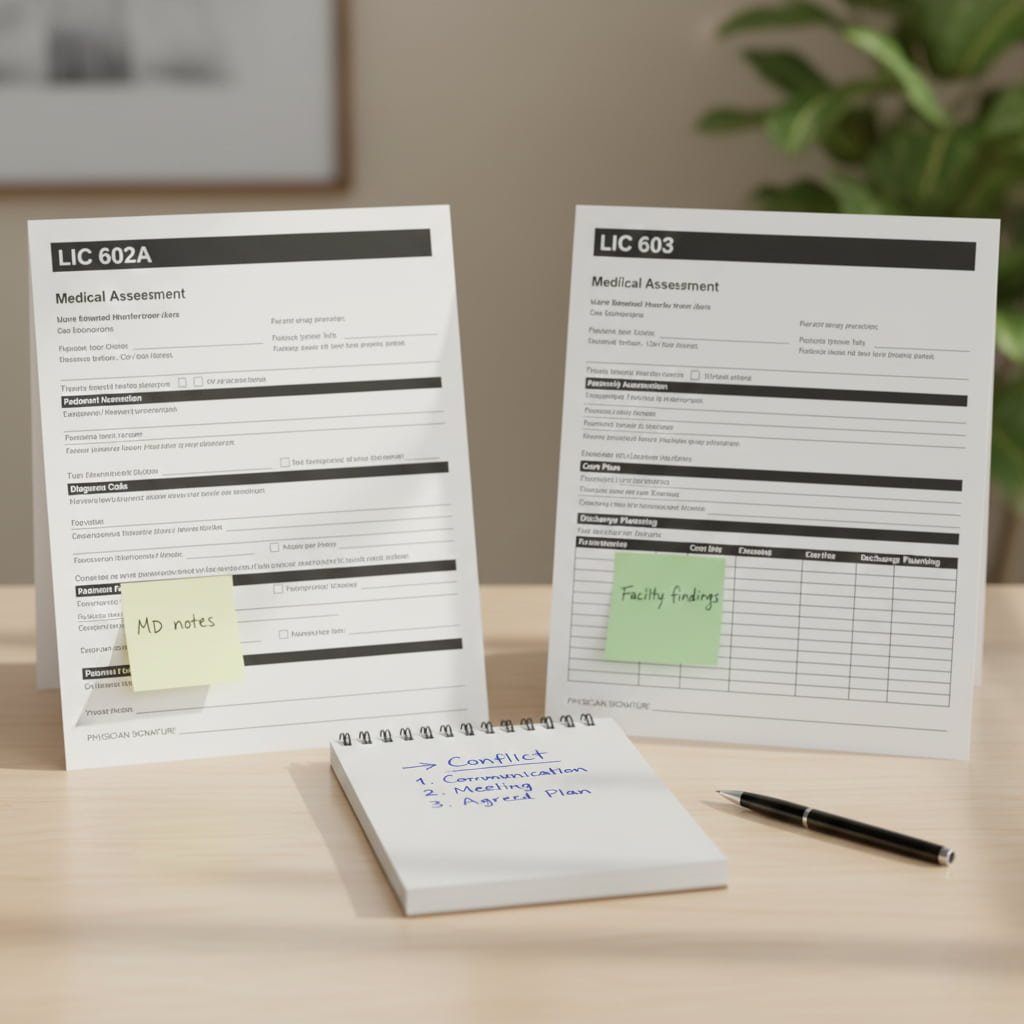
602A vs. 603: Aligning Physician and Facility Assessments
Image generated with AI for illustrative purposes only.
The Importance of Aligned Records for Your Care
In healthcare settings, such as long-term care facilities or rehabilitation centers, documentation accuracy is the bedrock of safety and quality of care. Every entry serves as legal substantiation for the services provided. When records are aligned, patient safety and continuity of care are achieved, as all professionals operate under a unified, confirmed plan.
The Core Problem: The 602A and 603 Conflict
Two key forms frequently create documentation conflicts:
602A (From the Physician): The primary focus is on medical necessity. The physician records diagnoses, necessary medical interventions, and limitations.
603 (From the Facility): The primary focus is on functional status. Staff assesses the specific assistance the patient requires in daily living (e.g., mobility, cognitive function, self-care).
A Conflict occurs when the physician's record of a medical condition (e.g., "severe congestive heart failure causing weakness") does not find a clear reflection in the facility's assessment of assistance needs ("patient is completely independent").
Consequences of Misalignment
If these documents contradict each other, the repercussions can be severe. The facility may face issues during state inspections (as required by CMS regulations), leading to deficiencies, fines, and citations. Most importantly, unaligned data can result in care errors, as staff may underestimate the medical risks identified by the physician.
Understanding the Basics
What Do 602A and 603 Assess?
| Form | Completed by | Primary Focus |
|---|---|---|
| 602A | Your Physician | Confirmation of Medical Necessity (why treatment is needed). |
| 603 | Facility Staff | Assessment of Functional Status (what assistance is needed for daily life). |
Why Alignment is Required for Oversight
Regulatory bodies require that all medical services be substantiated from both a clinical (physician) and a functional (facility) perspective. Discrepancies in the documentation can signal a failure to meet care standards or a lack of justification for the services being provided.
Discrepancies: Physician vs. Facility Perspectives
Conflicts arise due to the differing workflows and priorities of both parties.
Challenges on the Physician's Side
Physicians often work under time constraints and heavy workloads. This can lead to incomplete or abbreviated records that are difficult for facility staff to interpret. Furthermore, if the EHR (Electronic Health Record) systems used by the physician's clinic and the facility do not communicate, critical information may be delayed or missed.
Challenges on the Facility's Side
Facility staff completing the 603 form can face difficulties:
Misinterpretation of Clinical Records: Complex medical terminology or abbreviations used by the physician can be misinterpreted, leading to an inappropriate assessment of the patient's needs.
Incomplete Observations: The assessment of functional status may not fully capture all patient needs, especially cognitive impairments or the requirement for supervision.
Root Causes of Conflicts: Communication and Timing
According to NIH research, communication gaps among healthcare professionals are a frequent cause of medical errors. These gaps manifest in two key areas:
1. Differences in Terminology and Focus
Physicians typically focus on diagnosis and treatment, using clinical terminology (e.g., "significant hypotension"). Facility staff must translate this into functional needs ("requires assistance getting out of bed due to dizziness").
Example: If a physician only writes "chronic pain," the facility may assess the patient as fully mobile, unless the physician clarifies that the pain necessitates assistance with ambulation.
2. Synchronization Issues
CMS requirements mandate that medical documentation, including physician signatures, must be timely. If a physician signs or finalizes the 602A form late, it can create a mismatch with the 603 assessment, which may have been performed earlier, questioning the currency of the care plan.
Practical Strategies for Preventing Conflicts
To avoid discrepancies, facilities must focus on structured communication and education.
Standardizing Communication
There needs to be a shift from informal phone calls to formalized channels.
Collaborative Rounds: Establishing regular, structured meetings where the physician and key facility staff jointly discuss and reconcile patient status and the care plan.
Clear Requests: Utilizing standardized forms to request specific clarifying information from the physician regarding the patient's functional limitations.
Education and Technology Integration
Physician Education: It is essential to train physicians on how their clinical notes must be detailed enough to substantiate the patient's functional needs captured in the 603 form.
EHR Integration: Where possible, utilizing integrated electronic systems that can automatically compare key data fields between the two forms and generate real-time alerts when a conflict is detected.
Correcting Existing Errors
If a discrepancy is already identified (e.g., during an internal audit), a clear protocol must be followed:
Identification: Clearly pinpoint the point of divergence.
Joint Review: The physician and facility staff meet to align on the patient's current clinical and functional status.
Making Amendments: An amendment is made to the appropriate document.
CMS Requirements: Any addendum or correction must be dated with the current date and include a clear explanation of the reason for the change to maintain documentation transparency.
Example of Proper Alignment
Scenario: Physician wrote: "Patient with dementia. Needs supervision." The Facility recorded: "Patient is fully independent."
| What Went Wrong | How It Looks in Aligned Documentation |
|---|---|
| Discrepancy: Risk was incorrectly assessed. |
Physician (602A) clarifies: "Requires supervision due to short-term memory loss, creating a risk for skipping vital medications."
Facility (603) corrects: "Requires constant staff supervision to monitor medication adherence, as confirmed by physician documentation, to ensure safety." |
The Role of Audits in Maintaining Quality
Regular internal reviews (audits) of documentation are crucial for long-term success. They help identify systemic issues and inconsistencies before they are noticed by an external regulator. Thus, audits not only ensure compliance but also serve as a tool for continuous quality improvement in care.
Conclusion
Aligning the 602A and 603 documents is a fundamental requirement for ensuring patient safety and quality of care. Success requires bridging the communication barriers between clinical and administrative staff. By implementing standardized processes, educating personnel, and utilizing technology, facilities can ensure documentation accuracy and provide patients with the most consistent and safe care possible.
List of References and Resources
Centers for Medicare & Medicaid Services (CMS) – Documentation requirements for long-term care and skilled nursing facilities (SNFs); regulations regarding the timeliness, completeness, and legibility of physician orders and documentation; requirements for substantiation of services provided (CMS F-Tags related to physician services and quality of care).
National Institutes of Health (NIH) – Research on patient safety, quality improvement, and medical errors; studies highlighting communication gaps and poor teamwork as root causes of adverse events in healthcare settings; the importance of interdisciplinary collaboration.
Centers for Disease Control and Prevention (CDC) – General requirements for accurate medical records related to public health and infection control (e.g., data utilized in the NHSN system); guidelines supporting the need for consistent patient data to inform infection prevention and epidemiological tracking.
Mayo Clinic / Kaiser Permanente Division of Research – General principles of clinical documentation, ensuring consistency and continuity of care across different settings; research reinforcing the importance of clear clinical reasoning in medical records.